TMJ / TMD Overview
Please review this brief overview of Temporomandibular Joint Dysfunction
and then call our London, Ontario office to schedule your initial TMJ Consultation.
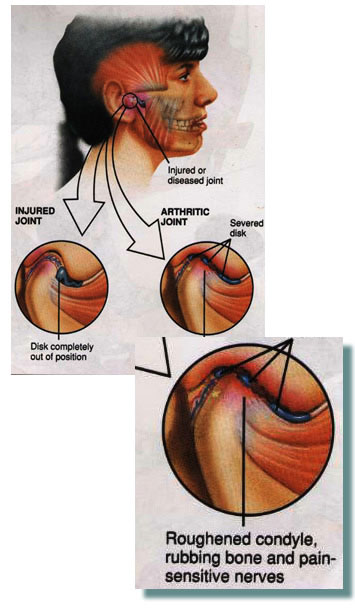
The temporomandibular joint (TMJ) is a ball-and-socket joint that connects the lower jaw (mandible) to the skull (temporal bone). The “ball” of the lower jaw bone, the condyle, fits into the “socket” of the temporal bone, or glenoid fossa, and the entire joint is surrounded by muscles and ligaments that work together to keep the lower jaw in the correct position. A piece of cartilage called an articular disc acts as a cushion or shock absorber between the two bones.
NORMAL JAW JOINT
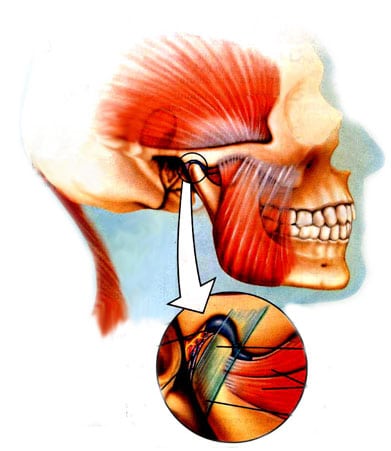
When the joint is healthy, the disc stays between the condyle and the glenoid fossa of the temporal bone at all times when the lower jaw opens and closes, allowing the patient to open wide without any discomfort or noise. (With a normal opening, the patient should be able to get three fingers between the upper and lower front teeth when the mouth is open as wide as possible.) A correctly functioning TMJ also keeps the muscles of the head, neck and shoulders function relatively pain-free.
What is TMD? (TMJ Overview)
Temporomandibular disorder (TMD) occurs when one or more aspects of the jaw don’t function properly. The position of your teeth, for example, is one factor that can affect the position of your jaw joints. Dental conditions like a deep overbite, a lower jaw that’s too far back, a narrow upper jaw or upper front teeth that are crooked or tipped backwards can cause the jaw to become dislocated, sending the disc too far forward and the lower jaw too far backward. As a result, the top of the lower jaw presses on the nerves and blood vessels at the back of the socket causing pain. Losing the cartilage between jaw bones can also lead to osteoarthritis.
Usually, the protective disc (cartilage) is displaced forward and no longer serves as a cushion between the condyle (lower jaw) and the bony socket (skull) and eventually this can lead to the condyle rubbing against the bony socket. This can cause a problem called osteoarthritis.
What’s that popping sound in my jaw?
Various noises within the jaw joints, such as clicking and popping sounds, happen when the disc becomes displaced and typically signal a displacement or dislocation of the jaw joint. It can be a painful condition that gets progressively worse, so patients are encouraged to seek treatment as soon as possible.
Over time, severe displacement can cause permanent joint damage, leading to an unstable bite and muscle strain and pain. Collectively, these symptoms may be referred to as craniomandibular dysfunction.
Mild displacements Cause Clicking or Popping Sounds in the Jaw Joint
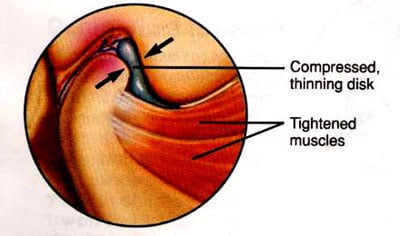
Photo of Degenerative Joint Disease and Degenerative Joint
Questions about TMJ & TMD?
INTERNAL DERANGEMENT OF THE TMJ
- Internal derangement indicates problems within the TMJ (jaw joint). This occurs frequently when the patient jaw is located too far back. There is noise or vibrations within the temporomandibular joints when the patient opens and closes and bites on the back teeth. This frequently means that the jaw is dislocated because the cartilage or disc is dislocated anteriorly or medially (sideways). This occurs frequently when the patient’s jaw is located to far back and close to the ear. The ideal treatment would be to wear a daytime orthotic (splint) to try and recapture the dislocated disc. Research has shown that if the disc can return to its normal position this can eliminate as many as 94% of the painful symptoms of TMD (TMJ).
EXTERNAL DERANGEMENT OF THE TMJ
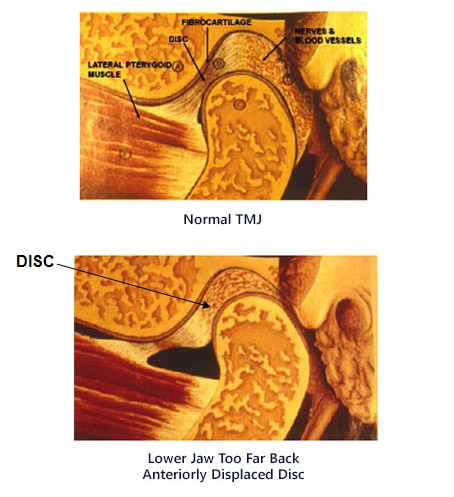
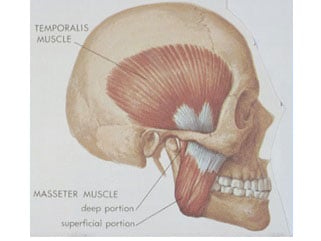
- External derangement indicates a problem outside of the TMJ or jaw joint which occurs when the muscles of the head and neck are sore as the result of the patient clenching and grinding their teeth, mainly at night. The resulting pain can be anywhere in the head and neck and mainly from the overuse of the temporalis muscle (temple area) and the masseter muscle (side of face) are as seen on the diagram.
- If the patient clenches and grinds their teeth at night while sleeping, the solution would be to wear a special night appliance to prevent this problem.
- The way the patient bites their teeth together or chews can cause interferences which can trigger painful muscle spasms. Treatment would involve adjusting the bite with a special device called a T-Scan.
At the initial consultation appointment efforts are made to determine whether or not the patient has symptoms which could be related to TMD (temporomandibular Dysfunction).
To help determine if the lower jaw and the discs of the TM (temporomandibular) joints are in the correct position the following diagnostic tests are utilized:
- Medical and Dental History as well as an examination of the teeth and the dental arches
- TMJ Health Questionnaire – Patients are asked questions regarding possible TM dysfunction symptoms. If the patient answers “yes” to any of the symptoms and “yes” to clenching and bruxing, then further tests are required to confirm the presence of a jaw joint problem (TM disorder). Some common TMJ symptoms include headaches, sore neck, earaches, ringing in the ears, stuffiness in the ears, dizziness, fainting, tingling in the hands and arm.
- Range of Motion – Patients will be examined for how wide they can open, move the jaw to the left and right, move the jaw forward, and whether or not when they open does their jaw open straight or moves to the right or left upon opening. If there is a problem achieving a normal range of motion, there is usually a structural problem within the joint.
- Muscle Exam – The muscles of the head and neck are extremely sore when examined if the patient is clenching and grinding all night. These muscles will be examined by Dr. Rondeau at the first appointment to determine the seriousness of the jaw joint problem. These muscles will be examined throughout treatment. When the muscle soreness is decreased this is an indication that the treatment has been successful.
- TMJ X-RAYS – TMJ x-rays (tomogram x-rays) are important to see if the condyles (top of the lower jaw bone) are too far back, when the patient bites on the back teeth, where they would be impinging on the nerves and blood vessels at the back of the socket. In cases where the lower jaw is too far back, we find a significant reduction in the signs and symptoms of TM disorders when the jaw is repositioned forward with a splint or a functional orthopedic appliance.
- COMPUTERIZED JOINT VIBRATION ANALYSIS (JVA) – When the joints of the body, including the TMJ or jaw joint are functioning normally there should be no noise or vibrations.
This is specialized equipment used to take readings of the noises or vibrations occurring within the jaw joints upon opening and closing movements. The JVA is simply a 3-minute, non-invasive test where headphones are placed on both jaw joints and the patient is instructed to open and close six times. An abnormal or dislocated joint has distinctive vibrations which can be analyzed to help diagnose the seriousness of the problem.
There are basically 5 stages of disc displacement. Ideally, if there is a jaw problem you would hope that the patient is in Stage 1 or Stage 2 where the disc can be returned to its proper position when the patients wear a lower repositioning splint during the daytime. If the JVA reveals that the patient is in Stage 3, 4 or 5, this is a much more serious problem and the prognosis is not as good for the resolution of all the symptoms.

Treatment
Phase One Treatment 4-6 months Jaw Stabilization Phase
Objective, Stabilize the TMJ and eliminate the symptoms.
The first goal is to relieve the muscle spasms and pain as well as establish a normal range of motion of the lower jaw. Our office utilizes a conservative non-surgical approach to treat patients with TMJ (jaw joint) problems. When the patient’s jaw is dislocated by the fact that the patient’s jaw makes a noise such as clicking or popping on opening or closing then the patient is instructed to wear the following orthotic splints or mouthguards:
- Daytime Orthotic (Lower splint) – The patient is instructed to wear a lower orthotic which is worn over the lower back teeth all day even while eating. This lower orthotic is made with grooves on the top surface so the patient can only bite down in one position. This position is determined by Dr. Rondeau and he instructs the dental lab to make the splint in a position where the jaw joint does not make a noise when opening and closing into the orthotic or splint.. The objective is to move the lower jaw forward the have the disc go back to its correct position. In other words, correct the dislocated jaw problem. When the jaw dislocation is corrected this eliminates most of the TMJ pain and discomfort. Many patients come to Dr. Rondeau’s office wearing a flat plane upper night guard that has been made by their dentist. This flat upper or lower nightguard cannot successfully fix the dislocated jaw problem. In fact, many times with the upper flat design nightguard the patient’s jaw moves farther back which makes the problem worse. In fact, sometimes the use of a flat nightguard on a patient whose jaw clicks can cause the jaw to lock (Lock Jaw is very painful).



- Nighttime Orthotic (Splint) – Many of our patients have a habit at night of clenching or grinding their teeth. This causes very sore muscles in the head and neck. To solve this problem Dr. Rondeau has designed a special night appliance which helps prevent this problem The upper orthotic (splint) is designed so that only the lower four front teeth contact this night appliance. Experience has taught us that if the back teeth do not touch when the patient tries to swallow then it is very difficult to clench and grind their teeth at night. When the back teeth do not contact during swallowing this will also significantly reduce headaches, particularly morning headaches.

Once the pain is under control and the jaw joint stabilized after 4-6 months the patient then has several options:
- Sometimes the disc will stay in position without the lower orthotic and the treatment has been successful and the patient no longer has to wear the lower orthotic. This is more common when the patients dislocated jaw is caused by a traumatic injury or a motor vehicle accident.
- If finances are a concern the patient is encouraged to keep wearing both day and night orthotics (splints)
- Some patient may wish to proceed to Phase 2 (Permanent Solution):
- Most patients prefer to consider orthodontic treatment for a short period of time, 12-18 months. The adult patients often choose clear braces which are extremely aesthetically pleasing (invisible braces). The space between the back teeth is then systematically closed with no discomfort when the patient wears elastics or rubber bands except when eating. After the teeth have come together holding the TMJ (jaw joints) in the correct position this usually means the patient is pain-free and the treatment has now been successfully completed. This is a permanent solution to the problem.
- If the space between the back teeth is very small after Phase I Orthotic treatment then some patients may want to consider crowns on the lower teeth. This may also be a viable option if the patient has extremely large fillings or missing teeth on the lower arch.
- Complete Dentures: If the patient wears complete dentures the solution might be to remake the dentures now that the TMJ is in the correct position.
- Lower Partial Denture: Sometimes making the teeth longer on the lower partial denture may be a possible solution.
TREATMENT OF PATIENTS WHO GRIND THEIR TEETH AT NIGHT
Grinding at night also known as bruxism is a very common habit. Signs would include the wearing down on the front and the back teeth. Also, defects along the gum line know as abfractions are signs of grinding at night. The solution would be to wear a special night appliance which helps prevent the problem.



TREATMENT OF PATIENTS WHOSE BITE CAUSES PAINFUL SYMPTOMS
Sometimes how the teeth come together when the patient bites can cause muscle spasms, headaches, earaches and other painful symptoms as described earlier. If the jaw moves side to side or forward there are interferences these sometimes cause muscle spasms and pain. These patients need to have a bite adjustment to correct the problem.
In our office, we use the most advance laser therapy system to offer our patients a painless, drugless, non-invasive way to help you recover from painful conditions.
MLS Laser therapy uses a patented multiwave, fully robotic laser to significantly reduce pain and inflammation while also promoting soft tissue repair.

For more information on TMJ and TMD in London, ON area call Dr. Rondeau and Associates at 519-455-4110!